Maternal mortality remains a pressing issue in the United States, where preventable pregnancy-related deaths account for a staggering percentage. With the nation leading its high-income peers in maternal mortality rates, urgent reforms in maternal health are essential to reduce these alarming figures. Recent studies reveal that a significant portion of these deaths could be avoided with better prenatal and postpartum care, as well as effective management of pregnancy complications. Additionally, racial disparities in healthcare magnify these challenges, affecting communities disproportionately. Addressing maternal mortality not only demands a systemic overhaul but also a commitment to equitable healthcare practices for all mothers.
The alarming rise in maternal mortality, often defined as deaths due to complications related to pregnancy, reveals an urgent public health crisis. This issue encompasses a variety of pregnancy complications, and its implications extend well beyond immediate childbirth experiences. Evaluating the outcomes related to maternal health highlights the need for enhanced postnatal care and awareness of persistent racial inequities in healthcare access. As we explore the consequences of these statistics, terms like ‘pregnancy-related deaths’ and ‘postpartum health’ serve as crucial focal points in our understanding of the broader issue at hand. By tackling these challenges with informed and inclusive policies, we can work towards a future where no mother is at risk of death during or after pregnancy.
Understanding the Rise of Maternal Mortality Rates
Maternal mortality rates in the U.S. have been a growing concern, with the country leading among high-income nations. Recent studies revealed a troubling trend: between 2018 and 2022, there was a notable increase in pregnancy-related deaths, primarily driven by factors such as systemic healthcare inequities and insufficient postpartum care. The findings underscore the fact that over 80 percent of these deaths are preventable, which raises questions about the effectiveness of the current healthcare policies and the access to maternal health services, especially for marginalized communities.
Critical to understanding this rise is the role of chronic conditions prevalent in pregnant individuals. Many women are experiencing serious medical issues such as hypertension and cardiovascular diseases at younger ages, which significantly contributes to the increased mortality rates. The data shows that American Indian and Alaska Native women face alarmingly higher maternal mortality rates compared to white women, highlighting the urgent need for targeted interventions to address these racial disparities in healthcare.
The Impact of Racial Disparities on Maternal Health
Racial disparities have consistently plagued the American healthcare system, particularly regarding maternal health. The stark differences in maternal mortality rates among racial groups are alarming—American Indian and Alaska Native women suffer the highest rates, which are nearly four times greater than those of white women. Such disparities emphasize a long-standing issue within the healthcare infrastructure that reflects systemic bias and discrimination, impacting access to quality prenatal and postpartum care.
Efforts to bridge these disparities have surfaced over recent years, but progress remains slow. Innovations aimed at reducing inequities, such as community-based programs and improved educational resources, have had limited impact on a national scale. To truly address these racial disparities, healthcare policies must be re-evaluated and adjusted, ensuring equitable access to safe pregnancy care for all women, regardless of their racial or socio-economic background.
Preventing Pregnancy-Related Deaths Through Improved Care
Preventing pregnancy-related deaths is not only about improving immediate healthcare services during pregnancy but also about addressing the entire continuum of postpartum care. Many deaths occur post-delivery due to complications that are often overlooked when short-term healthcare focuses on the initial weeks after birth. Developing comprehensive care strategies that include extended monitoring and support during the postpartum period can significantly reduce mortality rates.
The focus on such extended care is crucial—data shows that late maternal deaths, occurring between 42 days and one year postpartum, accounted for nearly a third of all maternal fatalities. A more inclusive understanding of the postpartum phase, recognizing it as a critical health period rather than an arbitrary timeline, can lead to better outcomes. Investing in public health infrastructure to enhance care during this time is essential for achieving the goal of reducing maternal mortality rates.
Addressing Pregnancy Complications and Healthcare Inequities
Pregnancy complications, especially those linked to chronic diseases, have a significant impact on maternal mortality rates. Conditions such as severe hypertension, cardiac disorders, and other complications are increasingly affecting younger women, amplifying the risks during and after pregnancy. The shift in the leading causes of maternal death, from hemorrhage to cardiovascular disease, necessitates a reevaluation of how these complications are treated and managed throughout pregnancy.
Moreover, the disparity in healthcare access plays a critical role in the outcomes of these complications. Women in underserved populations may lack access to necessary screenings and interventions that could identify and manage these conditions early. Implementing policies that prioritize comprehensive and preventative care is essential for reducing pregnancy complications and improving overall maternal health outcomes.
The Role of Public Health Infrastructure in Maternal Mortality
A robust public health infrastructure is vital to tracking and improving maternal health outcomes. The recent implementation of a national system for recording pregnancy-related deaths has provided valuable data but highlights how much work remains. With shifting healthcare policies and significant cuts in research funding, there are concerns about the sustainability of maternal health programs and their ability to effectively address the rising rates of maternal mortality.
To enhance this infrastructure, consistent funding and prioritization of maternal health initiatives are crucial. This includes advocating for comprehensive training for healthcare providers on the unique challenges faced by diverse populations, ensuring that preventive measures and quality care are accessible to all women. Only through a strong public health framework can we hope to reduce the alarming rates of maternal mortality and improve health outcomes for mothers across the nation.
Innovative Solutions for Postpartum Care
As maternal mortality rates continue to rise in the U.S., one area of focus must be innovative solutions for postpartum care. Many healthcare systems still adhere to outdated practices that only offer brief follow-ups weeks after delivery. Recognizing the importance of a longer-term recovery process, health systems need to implement models that prioritize ongoing support and surveillance of maternal health.
Emerging initiatives should look at integrating mental health support, chronic condition management, and education surrounding maternal care into postpartum practices. Programs that provide continuous support and resources can significantly help reduce late maternal deaths, ensuring that women receive the care they need well beyond initial postpartum check-ups.
Policy Changes for Better Maternal Health Outcomes
Addressing the rising maternal mortality rates requires critical policy changes aimed at improving maternal health outcomes. State-level policy variations significantly contribute to the disparities observed in maternal deaths across different regions. By analyzing successful models, such as those in California, other states can adopt similar approaches that prioritize equitable access to comprehensive maternity care.
Policymakers must focus on addressing systemic inequities and investing in public health initiatives that target pregnant individuals and families. Comprehensive policy changes must include funding for healthcare services, increasing the accessibility of preventive care resources, and supporting postpartum health programs. These changes could lead to substantial improvements in maternal mortality rates and overall maternal health.
The Importance of Community Engagement in Maternal Health
Community engagement plays a crucial role in improving maternal health outcomes and reducing pregnancy-related deaths. Grassroots organizations and local community groups can provide invaluable support by educating expectant mothers about healthcare resources, prenatal care, and postpartum health management. Empowering women through community-based programs helps to bridge gaps in healthcare access and supports marginalized populations.
Additionally, fostering strong connections between healthcare providers and local communities is essential for tailoring care to meet specific needs. Engaging community members in maternal health initiatives encourages feedback from those directly affected, allowing for services and programs that are more responsive to their needs. Ultimately, community-driven approaches can enhance maternal health outcomes and work toward reducing the disparities observed in maternal mortality.
Understanding the COVID-19 Impact on Maternal Mortality
The COVID-19 pandemic had far-reaching effects on healthcare systems globally, and maternal health was not exempt. The initial phase of the pandemic correlated with a rise in pregnancy-related deaths, reflecting how disruptions in healthcare access and resources impacted maternal care. As healthcare facilities prioritized COVID-19 response measures, many pregnant individuals faced delays in essential prenatal and postpartum care.
Furthermore, the pandemic exacerbated existing inequities in healthcare, particularly for marginalized populations who often have less access to comprehensive maternal health services. The implications of these changes underscore the need for more resilient healthcare frameworks that can respond to public health emergencies without undermining essential services like maternal care.
Frequently Asked Questions
What are the main causes of maternal mortality in the United States?
Maternal mortality in the U.S. is primarily caused by cardiovascular disease, which accounts for over 20% of pregnancy-related deaths. Other significant contributors include hemorrhage and pregnancy complications such as severe hypertension and eclampsia. These conditions are exacerbated by inequities in healthcare access and chronic health issues affecting women of reproductive age.
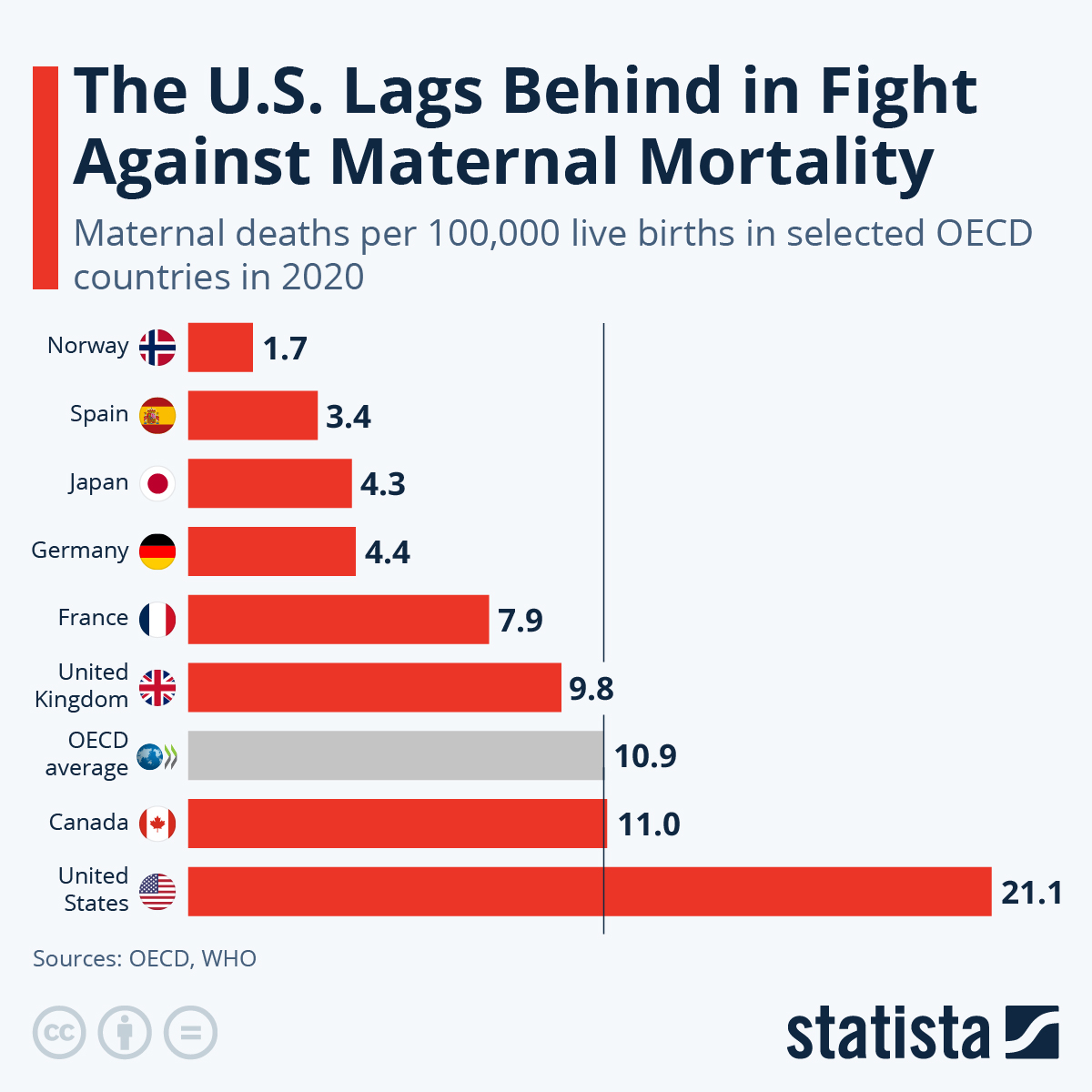
How does the U.S. maternal mortality rate compare to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries, with a rate of 32.6 deaths per 100,000 live births in 2022, up from 25.3 in 2018. This alarming trend reflects systemic issues in maternal health care, including disparities based on race and socioeconomic status.
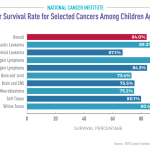
What are the disparities in maternal mortality rates among different racial and ethnic groups?
Significant racial disparities exist in maternal mortality rates, with American Indian and Alaska Native women facing the highest rates at 106.3 deaths per 100,000 live births, nearly four times that of white women, who experience a rate of 27.6. Non-Hispanic Black women also face high rates at 76.9 deaths per 100,000 live births, illustrating the urgent need to address these injustices in maternal healthcare.
Why is late maternal death significant in understanding maternal mortality?
Late maternal deaths, occurring from 42 days to one year postpartum, accounted for nearly a third of total pregnancy-related deaths in recent studies. Recognizing this period is crucial as it emphasizes the need for ongoing maternal healthcare support beyond immediate postpartum care, directly impacting long-term maternal health outcomes.
What can be done to reduce maternal mortality rates in the United States?
To reduce maternal mortality rates, there needs to be increased investment in public health infrastructure, improved prenatal and postpartum care, and policy changes addressing the disparities in maternal health. Innovative solutions that enhance access to quality care for all women, particularly in high-risk demographics, are essential for improving outcomes.
How do pregnancy complications contribute to increasing maternal mortality rates?
Pregnancy complications, such as severe hypertension and preeclampsia, significantly contribute to maternal mortality. These conditions are on the rise among younger populations, highlighting the need for better management and early interventions during prenatal and postpartum care to prevent fatalities.
What role does access to healthcare play in maternal mortality?
Access to comprehensive maternal healthcare directly impacts maternal mortality rates, with many deaths deemed preventable in areas lacking adequate healthcare services. Addressing maternity care deserts and ensuring equitable healthcare access across racial and socioeconomic lines are critical to reducing pregnancy-related deaths.
Why is the measurement of maternal mortality important for public health?
Measuring maternal mortality is vital for public health as it highlights gaps in care and identifies areas needing improvement. Understanding the dynamics of maternal deaths helps shape policies and practices that can effectively reduce risks and enhance overall maternal health outcomes.
| Key Points | Details |
|---|---|
| Rising Maternal Mortality Rates | The U.S. continues to have the highest maternal mortality rate among high-income countries, with a rise from 25.3 in 2018 to 32.6 deaths per 100,000 live births in 2022. |
| Preventable Deaths | Over 80% of pregnancy-related deaths in the U.S. are considered preventable. |
| Disparities by Race and Ethnicity | American Indian and Alaska Native women have nearly four times higher mortality rates compared to white women. |
| Leading Causes of Death | Cardiovascular disease is now the leading cause, accounting for over 20% of deaths. |
| Late Maternal Deaths | Late maternal deaths, occurring between 42 days and 1 year postpartum, comprise nearly a third of total deaths. |
| Need for Policy Changes | There’s a critical need to improve public health infrastructure and policies to enhance maternity care across states. |
Summary
Maternal mortality remains a pressing issue in the United States, where the maternal mortality rate is alarmingly high compared to other high-income countries. Recent studies indicate that significant improvements are necessary, particularly in preventive care and addressing racial disparities. With over 80% of pregnancy-related deaths being preventable, it is crucial to enact policies that prioritize maternal health and provide comprehensive postpartum care. The findings underscore a need for unified efforts to tackle the systemic issues contributing to these tragic outcomes.