Pediatric cancer recurrence is a pressing concern for families grappling with the emotional and physical toll of childhood cancers. A recent study has unveiled an innovative AI tool that excels in predicting the risk of relapse, particularly in pediatric patients with brain tumors known as gliomas. Unlike traditional methods, which often struggle with accuracy, this AI-driven approach analyzes multiple brain scans over time, enhancing the precision of predictions about potential cancer return. By leveraging advanced techniques in brain scan analysis, researchers are transforming the landscape of pediatric oncology, aiming for more tailored and effective treatment plans. This promising development heralds a new era of AI in medicine, where technology not only supports diagnostic capabilities but also seeks to improve patients’ quality of life through better prognostic insights.
The topic of childhood cancer relapse encompasses various synonymous terms, including pediatric malignancy recurrence and the challenges associated with managing these serious conditions. Children diagnosed with malignancies like gliomas face ongoing risks that can profoundly impact their recovery and future well-being. Innovative tools leveraging artificial intelligence are paving the way for enhanced risk assessment, particularly in forecasting cancer recurrence. The integration of advanced imaging techniques aids in understanding the complex dynamics of tumor behaviors and the probability of relapse, ultimately leading to improved strategies for monitoring and treating affected children. As the field evolves, the focus shifts towards creating more personalized care strategies that align with the unique challenges children face throughout their cancer journey.
Understanding Pediatric Cancer Recurrence
Pediatric cancer recurrence poses a significant challenge for both medical professionals and families. Unlike some adult cancers, which tend to follow more predictable patterns, pediatric cancers can behave erratically, presenting unique difficulties in their management. The recurrence can often lead to added distress for families who have already endured the initial treatment phases, which are themselves fraught with trials and tribulations. Parents and caregivers often seek answers to difficult questions regarding the risks and probabilities of recurrence, making this topic a critical area of research in the field of pediatric oncology.
Studies show that certain types of pediatric cancers, such as gliomas, have varying recurrence rates based on numerous factors including tumor type, treatment protocol, and individual patient responses. The ability to predict pediatric cancer recurrence more accurately can significantly influence treatment pathways, ultimately improving outcomes. Researchers are actively working towards developing advanced tools—such as artificial intelligence algorithms that analyze longitudinal imaging data— that can clarify and redefine relapse risks, providing a source of hope and more tailored treatment for these vulnerable patients.
The Role of AI in Predicting Cancer Relapse Risk
Artificial intelligence has emerged as a transformative force in the field of medicine, particularly in oncology, where it is being used to predict cancer relapse risk more effectively than traditional methods. AI systems can analyze the complex data obtained from multiple medical imaging scans, recognizing patterns and changes that may signal an impending relapse. This use of AI enhances clinical assessments, making it easier for healthcare professionals to understand patient trajectories and make informed treatment decisions.
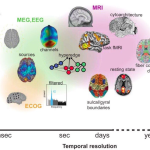
In recent studies, AI-driven approaches that implement techniques such as temporal learning have revolutionized how we examine brain scans in pediatric patients. By training AI algorithms with data collected over time, the tools learn to recognize subtle variations between scans that a human might overlook. The unprecedented accuracy of these tools offers possibilities to not only ascertain when a pediatric cancer is most likely to recur but to determine the most appropriate interventions earlier on, potentially leading to improved prognoses and quality of life for young patients.
Application of Temporal Learning in Pediatric Gliomas
Temporal learning represents a significant advancement in the analysis of pediatric gliomas, allowing for more precise assessments based on sequences of brain scans collected over time. Traditional AI models often relied on isolated images, which limited their predictive capabilities. Temporal learning, however, leverages the cumulative knowledge from numerous scans to discern trends indicative of cancer recurrence, leading to a more comprehensive evaluation of the patient’s status throughout their recovery journey.
Research has shown that this innovative approach not only increases prediction accuracy but also alleviates some stress from repeating imaging tests. By identifying which patients have a higher risk of relapse at an earlier stage, healthcare teams can conduct tailored imaging protocols, reducing unnecessary scans for low-risk patients while intensifying monitoring and treatment for those who require it. This model ensures a more organized and effective management plan, significantly alleviating the emotional and physical burdens on families.
Impact of AI on Pediatric Cancer Treatment Strategies
The integration of AI tools into pediatric oncology can have profound implications for treatment strategies. With improved accuracy in predicting cancer relapse, physicians can make more informed decisions regarding the frequency of imaging tests and the need for additional interventions. This targeted approach not only enhances patient care but also conserves precious healthcare resources that can be redirected towards more critical needs.
Moreover, insights gained from AI analysis could inspire the development of new therapeutic strategies—potentially pre-emptive, such as administering targeted therapies for patients identified as high-risk for relapse. This proactive stance could change the overwhelming trajectory of treatment for pediatric patients, providing a pathway toward better survival rates and an enhanced quality of life.
Future Directions in AI and Pediatric Oncology
Looking forward, the potential applications of AI technologies in pediatric oncology are virtually limitless. Current studies indicate that the algorithms developed for predicting relapse risk can extend beyond gliomas to encompass a wider range of pediatric cancers. This adaptability paves the way for more robust predictive models that can serve various patient populations across the globe.
As AI continues to evolve, ongoing clinical trials will be crucial for validating these tools and integrating them into routine practice. The future of pediatric oncology will likely be shaped by the extent to which AI can enhance diagnostic capabilities and treatment personalization, ultimately aiming to lower rates of pediatric cancer recurrence and alleviate the associated burdens on families.
Reducing the Emotional Burden of Monitoring
Monitoring pediatric cancer patients for potential recurrence often leads to emotional distress, not only for patients but also for their families. Frequent imaging, while necessary for tracking health trajectories, creates an atmosphere of anxiety and uncertainty that can be overwhelming. The recent advancements in AI, particularly with models that predict recurrence risks, can significantly alleviate this burden by reducing the frequency of unnecessary scans for patients with low relapse probabilities.
By allowing healthcare providers to focus resources more effectively, families can experience less disruption and anxiety. Lowering the frequency of imaging tests could help ensure that children spend less time in clinical environments and focus more on their recovery and quality of life, allowing them the opportunity to enjoy childhood without the constant reminder of their cancer journey.
Longitudinal Imaging for Enhanced Predictive Analysis
Longitudinal imaging—capturing a series of brain scans over time—plays an essential role in enhancing predictive analyses regarding pediatric cancer recurrence. By employing AI tools that leverage this rich dataset, researchers are able to identify persistent patterns that indicate potential relapses more effectively than with snapshot imaging approaches. The recurrent analysis build a more comprehensive understanding of each unique case, which is particularly vital in the context of pediatric patients where dynamics can shift rapidly.
This evolution of diagnostic procedures, anchored in robust AI methodologies, places greater emphasis on the significance of ongoing monitoring for pediatric cancer patients. It allows for a more nuanced approach to care plans, adjusting treatments based on the real-time assessment of their health status and risks, which is essential for optimizing outcomes in this vulnerable population.
Collaboration in Cancer Research Enhancing Outcomes
Collaboration between institutions, like that between researchers at Mass General Brigham and Boston Children’s Hospital, has proven essential in advancing knowledge on pediatric cancer recurrence. Such partnerships emphasize the value of shared expertise and resources in developing innovative solutions. By pooling their data and insights, researchers can accelerate the development of tools that precisely target patient needs, resulting in remarkably improved outcomes for those afflicted with complex conditions like gliomas.
These collaborative efforts are crucial not only for research but also for training the next generation of healthcare professionals in utilizing sophisticated AI technologies within pediatric oncology. As more institutions begin to integrate similar methodologies into their practices, the overall understanding and approach towards managing pediatric cancer recurrence will continue to advance, ultimately transforming patient care.
The Importance of Funding and Support in Cancer Research
Financial support from governmental agencies, such as the National Institutes of Health, is instrumental in enabling ground-breaking research in pediatric oncology. Studies such as those investigating AI applications in predicting cancer relapse risk require substantial resources to conduct extensive tests and validate findings. Securing funding ensures that innovative approaches can be explored and put into practice, potentially leading to breakthroughs in treatment methodologies and care.
Moreover, continuous investment in research fosters a culture of innovation and collaboration, motivating researchers to push the boundaries of what is achievable in medicine. As advancements in AI and machine learning technologies evolve, sustained financial backing will be crucial in translating these innovations into clinical applications that can significantly benefit the pediatric oncology landscape.
Frequently Asked Questions
How does AI influence the prediction of pediatric cancer recurrence risk?
AI plays a crucial role in improving the prediction of pediatric cancer recurrence risk, especially in conditions like pediatric gliomas. By analyzing multiple brain scans over time, AI can identify patterns and subtle changes that increase the accuracy of relapse predictions, thus outperforming traditional methods.
What are the benefits of using AI in predicting pediatric glioma recurrence?
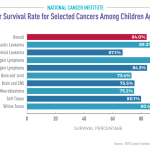
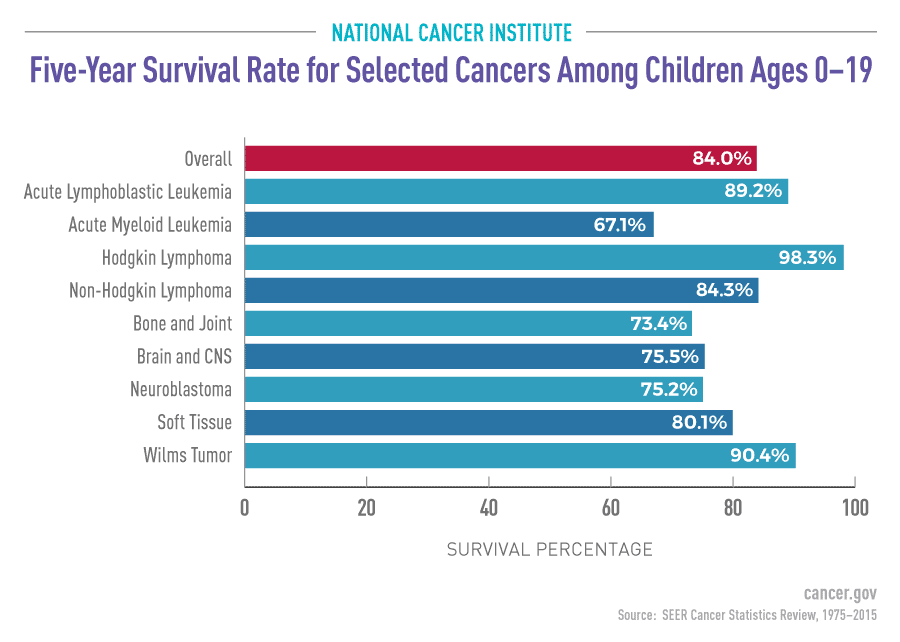
The use of AI in predicting pediatric glioma recurrence offers significant benefits, including higher accuracy in forecasting relapse risk. Traditional methods typically achieve only around 50% accuracy, whereas AI tools can reach up to 89% accuracy by utilizing data from multiple MR scans taken over time.
What is temporal learning and how does it relate to pediatric cancer recurrence prediction?
Temporal learning is a technique used in AI that analyzes a sequence of images over time to enhance prediction accuracy. In the context of pediatric cancer recurrence, it enables the AI model to detect changes in brain scans that may indicate a higher risk of relapse, particularly in pediatric gliomas.
How often should pediatric patients undergo imaging to monitor cancer relapse risk?
Traditionally, pediatric patients with a history of cancer, such as gliomas, undergo frequent imaging to monitor relapse risk. However, with advancements in AI, the frequency of imaging may be reduced for lower-risk patients, while high-risk patients can be identified for targeted therapies based on more accurate risk predictions.
What impact could AI have on the future management of pediatric cancer patients?
AI has the potential to revolutionize the management of pediatric cancer patients by delivering more precise predictions regarding cancer recurrence. This could lead to more tailored treatment plans, reducing unnecessary imaging, and improving overall care quality for children diagnosed with conditions like pediatric gliomas.
Why is it essential to improve tools for predicting pediatric cancer recurrence?
Improving tools for predicting pediatric cancer recurrence is essential to alleviate the stress and burden of continuous follow-up imaging on children and their families. Better predictive models can help identify those at highest risk for relapse, allowing for more focused and effective treatment interventions.
How do AI tools compare to traditional methods in predicting pediatric cancer relapse?
AI tools demonstrate a significant advantage over traditional methods in predicting pediatric cancer relapse. Research has shown that AI models can forecast recurrence with up to 89% accuracy through extensive analysis of multiple brain scans, dramatically surpassing the 50% accuracy commonly associated with singular image assessments.
What are pediatric gliomas, and why is monitoring their recurrence important?
Pediatric gliomas are a type of brain tumor that can often be treated successfully, yet they carry a risk of recurrence that can be serious. Monitoring their recurrence is crucial, as early detection can lead to timely interventions that may significantly impact a child’s health and treatment outcomes.
| Key Point | Description |
|---|---|
| AI Tool for Prediction | An AI tool offers more precise relapse risk predictions for pediatric cancer compared to traditional methods. |
| Focus on Pediatric Gliomas | Research emphasizes the importance of early detection of relapse risk for children with brain tumors. |
| Research Collaboration | The study involved multiple institutions, including Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. |
| Temporal Learning Technique | A novel approach using multiple brain scans over time to improve prediction accuracy of cancer recurrence. |
| Accuracy of Predictions | The AI’s predictions for recurrence reached an accuracy rate of 75-89%, outperforming traditional methods which were around 50%. |
| Future Clinical Trials | Plans to conduct trials to evaluate the practical application of AI in improving care for pediatric patients. |
Summary
Pediatric cancer recurrence is a critical focus in improving treatment outcomes for children with brain tumors. Recent advancements in AI technology have shown significant promise in predicting the risk of relapse more accurately than traditional methods. By utilizing a temporal learning approach with multiple MR scans, researchers can better understand and foresee potential relapses, which could lead to enhanced care and less frequent imaging for low-risk patients. The ongoing research aims to validate these findings through clinical trials, ultimately striving to transform pediatric cancer treatment.