In the realm of pediatric brain cancer, the emergence of AI in pediatric brain cancer is revolutionizing how we predict patient outcomes and manage treatment strategies. Traditional methods of predicting relapse risk have proven inadequate, making the integration of AI predictive tools vital for improving glioma prognosis among children. A groundbreaking study from Harvard indicates that specialized AI algorithms can analyze temporal changes in brain scans, offering unprecedented accuracy in forecasting brain cancer relapse. By leveraging vast datasets from pediatric patients, these advanced AI techniques promise to enhance the quality of care for children afflicted with this challenging condition. As the medical community moves toward embracing these innovations, the hope is to transform the daunting journey of managing childhood brain cancer into one that is informed and less stressful for families invested in their child’s health.
In the landscape of childhood oncological care, innovative technologies like machine learning are emerging as pivotal elements in effectively addressing brain tumors prevalent in young patients. The utilization of AI in pediatric brain cancer management is set to redefine approaches to monitoring and predicting patient relapse rates, integrating advanced algorithmic models that evaluate long-term imaging data. The focus on gliomas—common yet complex pediatric brain cancers—underscores the necessity of dynamic forecasting tools that adapt to shifting patient profiles. By applying concepts such as temporal learning, researchers are unlocking new dimensions in healthcare, allowing for tailored therapies that resonate with the unique challenges faced by pediatric patients. As the frontier of cancer treatment transforms, the synergy of AI and clinical practices holds the promise of significantly elevating outcomes for children grappling with the burden of brain tumors.
Understanding AI’s Role in Pediatric Brain Cancer Recurrence Prediction
Artificial Intelligence (AI) has emerged as a transformative force in medicine, particularly in the realm of pediatric brain cancer. In recent studies focusing on childhood brain cancer, AI predictive tools have demonstrated significant advancements in accurately forecasting relapse risks in young patients. Traditional methods often fall short due to their reliance on single scans and static data, but with AI’s ability to analyze longitudinal data, particularly multiple brain scans taken over time, clinicians can refine their risk assessments for patients diagnosed with gliomas, a prevalent type of pediatric brain tumor.
The integration of AI in understanding glioma prognosis has the potential to revolutionize patient care. Researchers have developed sophisticated algorithms that leverage temporal learning, allowing AI to track and interpret changes in brain scans across months. By identifying patterns that precede a recurrence, healthcare providers can initiate timely interventions, ensuring that patients at the highest risk receive preemptive care. This not only improves outcomes but also alleviates the emotional burden on families facing the uncertainties of cancer recurrence.
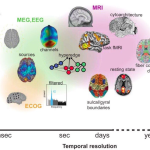
The Impact of Temporal Learning on Cancer Imaging
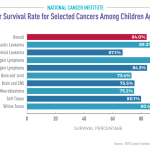
Temporal learning represents a paradigm shift in how medical imaging is conducted in oncology, especially for childhood brain cancers. Unlike conventional predictive models that evaluate individual scans, temporal learning enables the aggregation of multiple imaging over time, thus enhancing the accuracy of glioma prognosis. This innovative approach allows AI systems to recognize subtle fluctuations in tumor characteristics, which might indicate impending relapse. Encouraging, early results from studies indicate accuracy rates in predicting relapses ranging from 75% to 89%, far surpassing the near-chance predictions associated with non-temporal approaches.
Further advancements in temporal learning could lead to more personalized healthcare strategies in pediatric oncology. By systematically analyzing changes across a series of MRIs, AI not only provides a clearer picture of the patient’s status but also aids in determining the necessity and frequency of follow-up imaging. This could significantly reduce the emotional and logistical strain on young patients and their families, simplifying their journey through a complex and often tumultuous treatment landscape.
Challenges and Future Directions in AI for Pediatric Oncology
While the capability of AI to predict brain cancer relapse marks a significant milestone in pediatric oncology, several challenges remain. Chief among these is the need for further validation of AI predictive tools across diverse clinical settings. As illustrated in the study conducted by Mass General Brigham, thorough testing is imperative before these AI models can be applied universally in clinical practice. This includes ensuring that the accuracy observed in controlled environments translates effectively to real-world patient populations experiencing varied conditions and treatment protocols.
Moreover, establishing a framework for integrating AI insights into clinical workflows poses another hurdle. Oncologists will need to adapt to incorporating AI-guided risk assessments into their decision-making processes. Education and training will be essential to ensure that healthcare professionals can interpret AI findings effectively and communicate risks to patients and families. The hope is that as these AI tools mature, they will not only enhance glioma prognosis accuracy but also initiate a new era of proactive treatment for high-risk patients, potentially reshaping pediatric cancer care as we know it.
The Promise of AI Predictive Tools in Advancing Pediatric Cancer Care
AI predictive tools are making waves in pediatric oncology, particularly regarding the management of childhood brain cancer. These technologies offer immense promise for forecasting the likelihood of cancer relapse in young patients, particularly those diagnosed with gliomas. By analyzing vast datasets and identifying complex patterns across multiple MRIs, these tools improve clinicians’ ability to make informed decisions about treatment and patient monitoring.
Incorporating AI into the standard care framework could transform outcomes for children facing brain cancer. The potential to recognize relapse risks earlier in the treatment timeline allows for timely interventions, which can be crucial in mitigating the severe impact of recurrence on patients and their families. As researchers continue to refine these predictive models, the hope is to establish a new gold standard for monitoring and treating pediatric brain cancer that emphasizes not just survival but also quality of life.
Reducing Stress for Families through AI-Enhanced Monitoring
Navigating the complexities of childhood brain cancer can be an exhausting journey for families, with frequent imaging and follow-ups exacerbating stress levels. AI-driven monitoring solutions that accurately predict the risk of relapse may significantly alleviate some of this burden. Traditional follow-up protocols often require extensive imaging, leading to emotional and psychological strains for both children and parents. However, with enhanced predictive capabilities brought forth by AI, there’s a growing possibility of tailoring follow-up schedules based on each patient’s unique risk profile.
By identifying which patients are at lower risk for recurrence, healthcare professionals can space out necessary imaging sessions, rather than adhering to a one-size-fits-all approach. This not only reduces the frequency of MRIs but also gives families peace of mind, knowing that their child is being monitored in a way that is proportional to their individual needs. Overall, these advancements lead to improved psychological wellbeing for families, allowing them to focus on the healing process rather than the anxiety surrounding frequent medical visits.
Exploring Neurological Imaging Advances in Pediatric Brain Tumors
Advancements in neurological imaging technology are paramount in the field of pediatric brain cancer, particularly as they relate to ongoing research utilizing AI. Enhanced imaging techniques allow for a more detailed understanding of childhood brain tumors, aiding in the tracking of glioma progression and relapse risks. By leveraging AI’s capabilities in analyzing complex imaging data, researchers can gain deeper insights into tumor behavior over time, ultimately improving prognostic accuracy.
Beyond mere detection, these imaging improvements, combined with AI analysis, offer the potential for nuanced treatment options tailored specifically to a child’s individual tumor characteristics and response to therapy. In the future, we can anticipate a shift towards more adaptive treatment plans that will be guided not just by initial diagnoses but by real-time monitoring of tumor dynamics made possible through sophisticated imaging technology.
AI Innovations Transforming Clinical Trials in Pediatric Oncology
AI innovation is set to reshape clinical trial methodologies in pediatric oncology, particularly regarding predicting outcomes for childhood brain cancers. As researchers gather large volumes of data regarding glioma treatment responses, AI can streamline the identification of eligible patients for trials based on predictive analytics concerning their relapse risk. This targeted approach not only enhances trial efficiency but also ensures that experimental protocols align closely with patient needs.
Furthermore, AI’s predictive capabilities can support more adaptive trial designs, enabling the real-time modification of study parameters based on incoming data. This could lead to faster iterations of treatment approaches and ultimately pave the way for breakthrough therapies tailored specifically to pediatric brain tumors that are otherwise challenging to treat. The promise of AI in this capacity heralds a future where clinical trials can be more responsive to patient dynamics, increasing the likelihood of developing successful interventions for young cancer patients.
Bridging the Gap Between Research and Practice in Pediatric Brain Cancer
Bridging the gap between groundbreaking research and practical application is a pivotal challenge in the field of pediatric brain cancer treatment. While innovations in AI predictive tools offer immense potential for improving glioma prognosis, translating these findings into everyday clinical use requires thoughtful integration with existing healthcare frameworks. A coordinated strategy involving researchers, clinicians, and healthcare policymakers will be essential to facilitate this transition.
Additionally, ongoing education and training for healthcare providers on utilizing AI in their practice will help ensure that the benefits of these technological advancements reach the patient level. Collaborative efforts between institutions, including shared data and resources, could foster an environment conducive to innovation, enhancing the collective ability to combat pediatric brain cancer. By fostering partnerships that emphasize both scientific discovery and clinical application, it is possible to create a more effective and holistic approach to managing childhood brain tumors.
Long-Term Implications of AI on Pediatric Cancer Survivorship
The long-term implications of integrating AI into pediatric oncology extend far beyond immediate treatment outcomes. By improving the prediction of glioma relapse and tailoring monitoring protocols to individual risk profiles, AI has the potential to significantly enhance the survivorship experience for children with brain tumors. Reducing the need for frequent, invasive imaging and the emotional burden associated with it can contribute to a better quality of life as these young patients transition into survivorship.
As researchers continue to explore AI’s role in predicting and managing recurrence risks, the framework for long-term follow-up care is also evolving. Personalized care pathways developed with the input of AI insights can lead to improved health outcomes and foster a supportive network for ongoing management throughout a survivor’s life. Ultimately, as AI continues to advance in the context of pediatric brain cancer, it holds the promise for not only improved survival rates but also enriching the overall experience of childhood cancer survivors.
Frequently Asked Questions
How does AI improve outcomes in childhood brain cancer treatment?
AI in pediatric brain cancer enhances treatment outcomes by predicting relapse risks with greater accuracy than traditional imaging methods. A recent study revealed that AI tools could analyze multiple MRI scans taken over time, helping to identify children at the greatest risk of glioma recurrence early on. This predictive capability allows for better-tailored treatment strategies and aims to reduce the burden of frequent follow-ups.
What role does temporal learning play in AI predictive tools for glioma prognosis?
Temporal learning is crucial for AI predictive tools in pediatric brain cancer as it enables the models to analyze a sequence of MRI scans taken over time. This method allows the AI to recognize subtle changes in a child’s brain scans that may indicate a glioma relapse. By employing temporal learning, researchers have improved the prediction accuracy of recurrence risk significantly compared to traditional single-scan analyses.
Can AI tools help in reducing brain cancer relapse in pediatric patients?
Yes, AI tools are designed to predict the risk of brain cancer relapse more accurately in pediatric patients with gliomas. By analyzing multiple brain scans over time, these AI systems can identify high-risk patients who may require closer monitoring or preemptive treatments, potentially reducing the chance of recurrence and improving overall outcomes.
What are the benefits of using AI in monitoring childhood brain cancer relapse?
Utilizing AI in monitoring childhood brain cancer relapses offers several benefits, including improved accuracy in predicting which patients may experience a recurrence. This allows for more personalized follow-up care, decreases the frequency of unnecessary imaging in low-risk patients, and enhances the overall management of gliomas, ultimately leading to better quality of life for affected children and their families.
What findings did the study on AI in pediatric brain cancer reveal about glioma prognosis?
The study highlighted that AI in pediatric brain cancer could predict glioma prognosis with an accuracy of 75-89% for recurrence within one year post-treatment. This significant advancement over traditional methods, which only achieve about 50% accuracy based on single images, showcases the potential of AI tools to transform how clinicians monitor and intervene in pediatric brain cancer cases.
| Key Point | Description |
|---|---|
| AI Tool Effectiveness | AI predicts relapse risk with greater accuracy than traditional methods. |
| Study Participants | Nearly 4,000 MRI scans from 715 pediatric patients were analyzed. |
| Temporal Learning Technique | AI trained on multiple scans over time achieves better predictions than single scan analysis. |
| Prediction Accuracy | The temporal learning model predicts recurrence with an accuracy of 75-89%. |
| Clinical Implications | Further validation needed before applying AI in clinical settings, with potential for reduced imaging frequency for low-risk patients. |
Summary
AI in pediatric brain cancer is revolutionizing how doctors predict relapse risk in children with brain tumors. The research conducted at Mass General Brigham has demonstrated that an AI tool utilizing temporal learning can significantly enhance the accuracy of predictions regarding cancer recurrence, outperforming traditional single-scan methods. This breakthrough could potentially transform patient care by allowing for earlier intervention strategies and reducing the need for frequent imaging. As clinical trials are planned to further validate these findings, the hope is that AI can ultimately alleviate the burden on young patients and their families during follow-ups.